 |
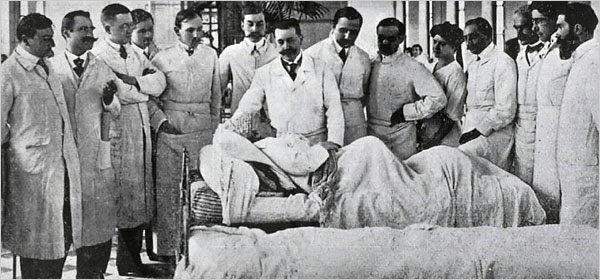
| Doctors practice “grand rounds,” ca. 1920s. (National Library of Medicine) |
This post is meant to provide a bit of background about how the day works and how a medical team functions so the references I make in future posts are clear. Let’s begin with the team. Nearly every medical team at an academic hospital consists of an attending physician, residents, interns, and medical school students. While these terms might sound familiar to anyone who has watched medical dramas on TV, it’s likely that most people don’t know what they mean. The attending physician is a bit like a tenured professor. He or she has the most experience and training in the operating room and the clinic, and has graduated from medical school, residency, and, in most cases, a fellowship program.
The residents, having graduated from medical school, are also physicians but, being less experienced, are “attendings-in-training,” learning the craft of a specialty via instruction from an attending physician. Residents are classified by the number of years they’ve spent in training, and different specialties will require a shorter or longer residency: there are chief residents (the most experienced residents), fourth-year residents, third-year residents, and so forth. Then there are the interns, physicians who have just finished medical school and are spending their first year out of school rotating through different specialties, learning how to enter orders for medications, writing progress notes on patient care and discharge notes to release patients from the hospital, and responding to immediate issues that arise during the course of the day. To do this an intern must know each patient in order to respond to questions about treatment from the patient and nurses.
Third-year medical students comprise the lowest rung of this ladder. We have little to contribute and plenty to learn. Frequently, we are assigned to follow a few patients and come to know as much as we possibly can about them. Once we know everything about our patients, it will be easier for us to think about what is most important regarding each patient’s care. We learn to pay attention to important details.
This team hierarchy, though it may seem stilted, is actually integral to the process of rounds, where the medical team visits each patient in its care. Rounding provides an opportunity for the healthcare team to speak with patients about how they are doing, to look at and physically examine them. The physical part of the exam is fundamental to healthcare. The abdomen, for example, can feel distended or stiff if there is a certain pathological problem, such as a bowel obstruction. Only by palpating — touching the patient’s body — can we know this. One cannot assess a patient’s progress until one examines a patient.
There are two official times to round during the day. One is immediately upon arrival at the hospital without the attending physician. This involves residents and medical students. And the other is with the attending physician later in the morning. While shuffling between different floors and patients, the hierarchy remains eminently clear. The attending physician leads the charge and behind him or her follows, in order of experience, everyone else: the third-year, the second-year, then the interns, then the medical students. There are usually about eight of us rounding together; to an untrained observer, we might look like the motorcade of a foreign diplomat. We all squeeze into each patient’s hospital room as the attending physician conducts the interview with the patient, assesses the patient, and tells the patient what the team’s plan is over the course of the day: Will a new medication be prescribed? Will the patient finally be able to eat food? Can the patient only drink liquids? As the attending explains this to the patient, one of the interns runs over to the computer inside the patient’s room and enters in the new medication orders or dietary orders. And on to the next patient. Over the course of the day, the new orders are confirmed and reconfirmed with the attending and upper level residents,
This daily pattern of rounding is actually a tradition as old as the American hospital system itself. In earlier days, there was a system of apprenticeship. So, if you wanted to be a physician in late-eighteenth-century America, you would be apprenticed to a doctor who would teach you all that you needed to know. You would then probably be offered a partnership with your teacher. But as the hospital and medical school system took root in the early nineteenth century, students pursued learning opportunities in hospitals in order to receive a more thorough practical education en masse. Individual physicians, after all, had very little time to apprentice aspiring doctors, and frequently the knowledge you received depended solely on one person. In order to teach medicine, hospitals created special programs where students would, as they do today, pay a fee for a basic science education (meaning anatomy, physiology, and pathology) and, eventually, a clinical one as well. Students rounded with residents (also known as house staff) and attendings in order to receive this practical experience in patient care. One description of rounds in Massachusetts General Hospital by Dr. James C. White in the 1850s sounds eerily familiar to me:
[The attending physicians] pass from bed to bed in the large wards, the students following. The house [officer] narrates any incidents in each patient’s condition during the previous twenty-four hours; the physician asks questions, makes the necessary explanations, and directs treatment. Over new and interesting questions much time is spent…. Students have nothing to do with the investigation of cases; they have only to look and listen.
My theory about this process as an educational tool is that it is suited to the role of each member of the team. The upper-level resident should be learning how to dictate orders and take charge of the team because soon he or she will be in that position. The attending, who knows this process well, educates the upper-level resident on whether the plan of care is correct and guides the fourth-year or chief resident. The mid-level resident follows closely on the heels of the upper level because he or she will soon occupy that position. And the interns need to learn how to manage patient care on a detailed level, writing notes and orders to improve at compounding a ton of information into a paragraph or two and assessing doses and units of medications.
And we, the medical students, observe and listen and ask questions when we can. Our purpose is to learn the language by observing patterns in patient care and disease. Thus far, it’s difficult to tell whether this strategy is working; it sometimes feels like I am back in French class on the very first day, listening to a language I’ve never heard before regarding dosages, plans of care, boluses, IV infusion rates, and so forth. But it is also comforting to know that this process has worked for more than a century and a half, and so perhaps we third-year medical students are right where we should be.